Radiology uses various types of radiation to acquire images of the human body.
Firstly, radiology applies electromagnetic waves of various lengths. The following are used in practice:
* radio waves – in magnetic resonance (MR) imaging technique;
* X radiation, also referred to as Röntgen radiation – in X-ray imaging (radiography, fluoroscopy also dental imaging and mammography), angiography and computed tomography.
Secondly, radiology makes use of high-frequency sound waves, above the upper limit of human hearing. These are applied in medical ultrasound imaging.
Depending on the imaging technique, rays of the respective types are transmitted through the patient's body in different ways and then recorded and presented as an image of the body's internal structures. This is why radiology is referred to as a transmission technique.
If radiation causes ionisation of the medium through which it passes (it detaches at least one electron from a neutral atom or molecule), it is referred to as ionising radiation. X-rays represent this type of radiation.
Ionising radiation is absorbed by the tissues of the human body, potentially causing an adverse impact. This may take the form of either deterministic or stochastic effects. Exposure of the human body to ionising radiation is measured using the so-called effective dose, the unit of the measure being the sievert (Sv). The prefixes used in practice are: millisievert (1 mSv = 0.001 Sv) and microsievert (1 µSv = 0.000001 Sv). It is assumed that a single dose is low if it does not exceed 100 mSv. A large dose corresponds to exposure to a few or more Sv.
It is also assumed that exposure to a single dose up to 0.25 Sv leads to no clinical symptoms.
As regards the impact of ionising radiation:
* Deterministic effects are adverse responses of the body, possibly leading to health problems, and directly produced by ionising radiation. Radiological imaging examinations apply low doses of radiation and if the required ways of proceeding are followed, these do not produce such immediate effects. It has been shown that a single dose of up to 0.25 Sv does not produce the above responses.
*Stochastic effects lead to possible changes of mutagenic nature which potentially may result in development of cancer or heritable consequences.
When considering the risk of cancer in a large population where each member would be subjected to a single dose of 10 mSv, this theoretical risk would be approximately 1:710 - 1:1300 (BEIR data). To gain a proper perspective this value should be compared with a risk of death due to spontaneous cancer, which is estimated at about 1:4!
The fear of being exposed to ionising radiation (X-rays in radiology) is rather common. But what most of us do not realise is that while living on planet Earth, we are exposed to ionising radiation from many sources all the time. These are mostly natural sources - primarily radioisotopes from the Earth's crust (mainly radon, which we breathe) as well as cosmic radiation. Moreover, ionising radiation comes from the food and liquids we consume, as they contain natural radioactive isotopes (mainly potassium40).
According to UNSCEAR (United Nations Scientific Committee on the Effects of Atomic Radiation), in one year the statistical inhabitant of the Earth receives a dose of 2.4 mSv from natural sources. This is the so-called natural background radiation. In Poland, the dose is estimated at 2.45 mSv/year. However, there are places across the globe (inhabited by people) where the dose of background radiation is much higher, these include e.g. Ramsar in Iran, Guarapai in Brazil or Lodeve and Lauragais in France.
Additional doses received by the Earth's population come from sources related to human activity - for example, electronic industry, chemical industry, mining, power generation and last but not least, medical practice. In Poland, the so-called total effective dose (from natural and man-made sources) amounts to 3.35 mSv/year.
We are concerned about ionising radiation, but as we use air transport more and more, we overlook the fact that with increasing altitude, the dose of cosmic rays to which we are exposed during flight is also higher. At an altitude of 12,500 metres, the intensity of ionising radiation coming from space is 200 times greater than at ground level. But the dose we receive during a flight depends on the duration of the flight and also the route - exposure to cosmic rays increases at higher latitudes.
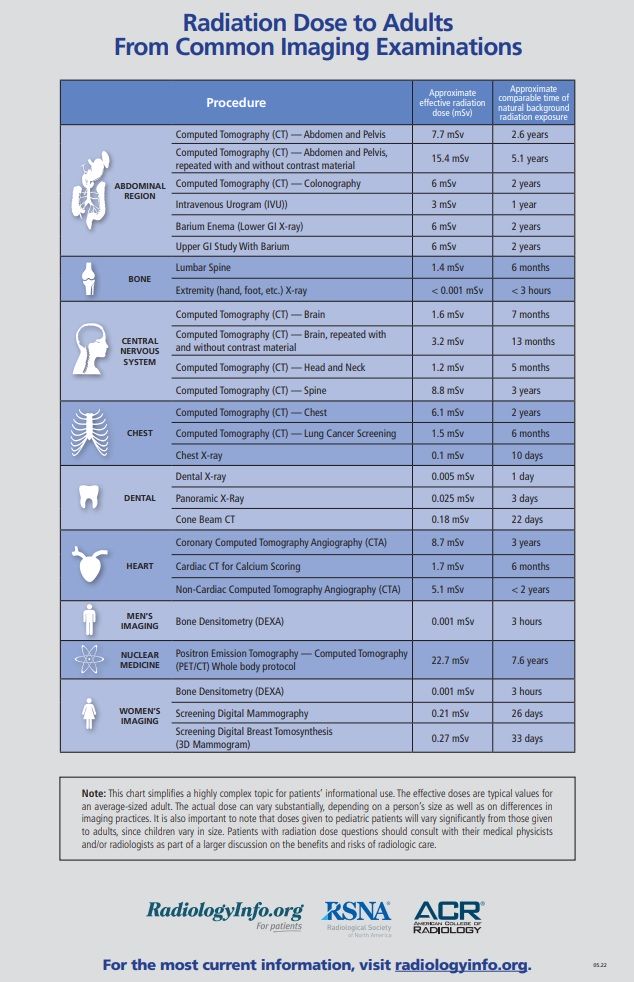
A statistical inhabitant of the Earth, over the course of a year, receives a radiation dose of 2.4 mSv from natural sources. Therefore, we should also know what effective doses are received during a typical radiological examination – see the chart below.
Although the risk of overexposure during radiological examinations is low, a number of procedures have been developed to control radiation doses. The guiding principle related to radiation safety is ALARA (acronym for As Low As Reasonably Achievable). It means that the required effects, i.e., useful diagnostic images, are to be acquired by using only the minimum doses of radiation which make it possible to accomplish the task. In other words, a higher image quality than required to make a diagnosis may be associated with the patient's exposure to an unnecessarily high dose. On the other hand, when insufficient radiation is applied, the image acquired may lack information necessary to make an accurate diagnosis. As a consequence, there may be a need to repeat the examination.
Radiological protection of the patient is a priority in radiology. It involves a series of operations and restrictions aimed at minimising a patient's exposure to ionising radiation, which will not unduly impede or prevent the acquisition of desired and well-founded diagnostic information or therapeutic effects (definition: Atomic Energy Act).
Presented below are the main principles applied in radiology to protect patients against ionising radiation.
1.
In the diagnostic process involving the use of ionising radiation, it is necessary to select an appropriate examination technique best suited to the clinical condition. Whenever feasible, techniques without the use of this type of radiation, or applying the lowest possible doses should be selected. When referring a patient for examination which applies ionising radiation, it is necessary to justify the decision and demonstrate that the benefits outweigh the risks and that alternative techniques without such radiation have been considered. If the patient was subjected to radiological examinations earlier, in order to perform these again, it is necessary to make sure that the earlier tests cannot provide sufficient information.
Various guidelines have been defined to make it easier to take the decision which type of examination is most suitable for a given patient. The most common are:
- iRefer: Making the Best Use of Clinical Radiology – 7th edition” eveloped by the Royal College of Radiologists (UK)
- ESR iGuide (Imagoing Referral Guidelines) by the European Society of Radiology
It should be emphasised that the final decision on the necessity and method of performing the examination is always made by the doctor, specialist in radiology.
2.
It is necessary to comply with all legal standards applicable in radiology - primarily the EURATOM directive and derived legislation.
3.
It is necessary design examination protocols for the specific patients rather than use the standard ("impersonal") procedures. For this purpose a medical professional specialising in radiology should be present during the examination. Only X-rays (including mammography and dental X-rays) can be performed by the radiographer alone.
4.
It is imperative to use only fully operational radiological equipment, complying with all standards, and certified to have achieved positive test and audit results. This also applies to other equipment used in radiological diagnostics - negatoscopes, monitors, automatic syringes, etc.
5.
Wherever necessary and possible, direct patient protection measures should be used. These can be lead-rubber aprons or special covers for specific organs (gonads, thyroid).
6.
Special protection should be provided to children and pregnant women. Foetuses and children are thought to be more sensitive to the effects of radiation than adults. The risk posed by radiation exposure during pregnancy depends on the stage of gestation and on the dose absorbed by the embryo or foetus.
The highest risks are associated with exposure to ionising radiation during the initial phase of organogenesis - between 3 and 8 weeks of gestation. Such exposure can cause birth defects (it is estimated that a realistic risk exists at doses exceeding 100 mSv). The risk decreases in the second trimester, and is lowest in the third trimester of pregnancy, but it should be remembered that the central nervous system, which is extremely sensitive to radiation, is developing rapidly between 8 and 25 weeks of gestation. Importantly, the risk of cancer induced by ionising radiation in foetal life and in children and adolescents is 2-3 times higher than the average risk (on the other hand, for people over 60 years of age the risk is lower; possibly about 5 times).
In view of the above, medical imaging procedures using ionising radiation should not be applied to pregnant women. An exception to this rule is when no alternative diagnostic techniques can be used and when the examination cannot wait until after the baby is born whereas the benefits outweigh the hazards. Also, such examinations are performed when the patient's life is at risk. The exposure of the unborn child to the radiation should then be minimised.
Owing to all these procedures, examinations carried out with the use of ionising radiation, if performed with appropriate equipment, in a correct way and for justified reasons, produce significant health-related gains for the patient that far outweigh the potentially existing, albeit small, risks.
The text was written in cooperation with the National Centre for Radiological Protection in Healthcare.


